First established in April 2020, the Global Fund’s COVID-19 Response Mechanism (C19RM) was designed to rapidly respond to the global health emergency created by SARS-CoV-2. Building on 20 years of experience in fighting three of the deadliest infectious diseases, and using its comparative advantages in procurement, deployment at scale and existing relationships with implementing countries and communities, the Global Fund was swiftly able to step up its COVID-19 response.
Since first establishing C19RM, the Global Fund has been able to expand, refine and develop the mechanism. It learned lessons and responded as the pandemic evolved and adapted to changing country needs and the availability of new tools such as self-testing and oral antivirals.
Through C19RM, the Global Fund has been the primary source of funding for all COVID-19 tools, except vaccines. Thanks to the generous backing of donors, the Global Fund has awarded over US$4.9 billion since March 2020 to 109 low- and middle-income countries (LMICs) and 22 multi-country programs, to support health and community health workers and communities fight and recover from COVID-19.
The Global Fund has been able to support LMICs in responding to the new virus, mitigating the knock-on impact on HIV, TB and malaria programs and protecting the health services. C19RM support included providing access to diagnostics, oxygen, therapeutics, and personal protective equipment (PPE) at a time of unprecedented global demand, as well as adapting lifesaving HIV, TB and malaria services and investing to reinforce overstretched health systems, including supporting community health workers.
In addition to provision of COVID-19 tools, countries were encouraged to invest in crucial Community interventions, such as responding to human rights and gender related barriers to services, community-led monitoring, community-led advocacy and research, social mobilization, building community linkages and coordination, institutional capacity building, planning and leadership development, and gender-based violence (GBV) prevention. Working through the community engagement strategic initiative partners, communities and civil society were able to access technical support to engage in the process.
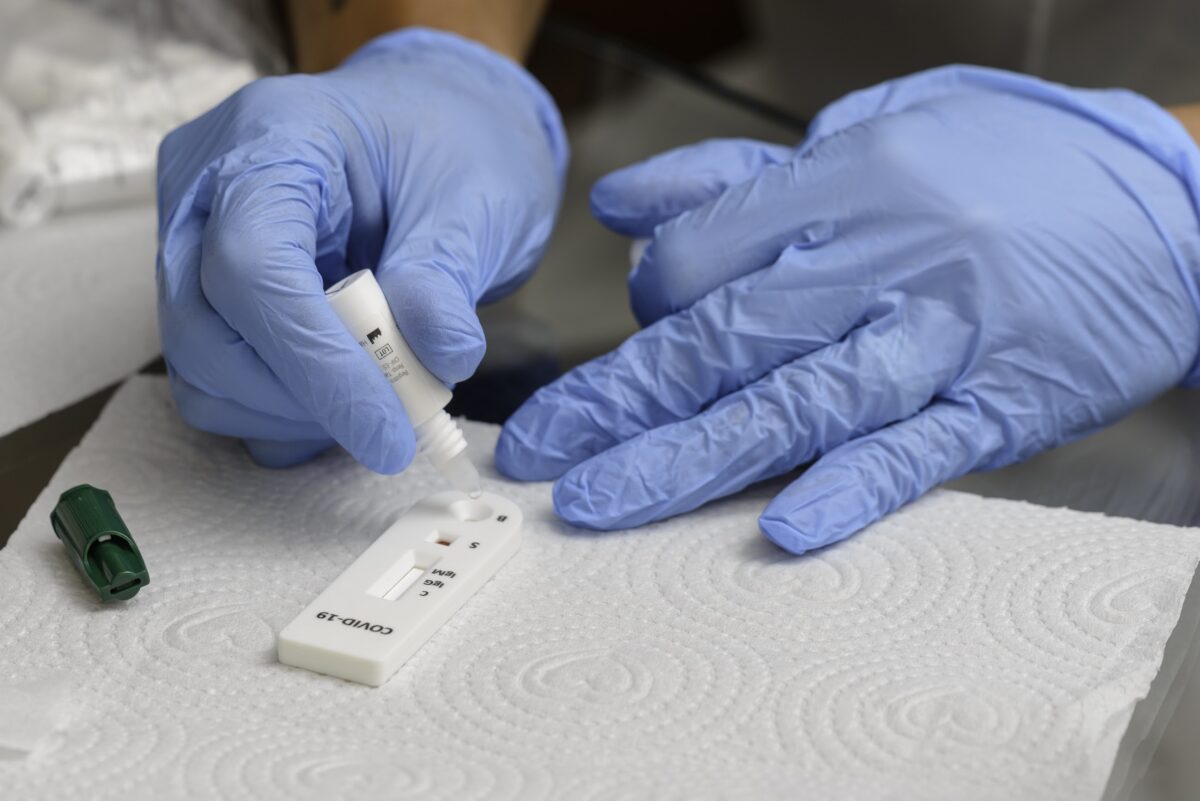
C19RM on Diagnostics
From the start of the pandemic, the Global Fund took a leading role in supporting LMICs to scale up testing for the new virus, based on 20 years of experience in procuring diagnostics and investing in laboratory capacities.
C19RM investments have backed countries’ efforts to address the acute difficulties in sourcing PCR and rapid antigen diagnostic tests (Ag-RDT) and scaling-up testing in response to COVID-19 – including supply-side constraints, high costs, quality issues, long delivery times and delays in the issuance of guidance on testing strategies. C19RM procured PCR tests and Ag-RDTs, strengthened laboratory systems and network capacities, and reinforced national testing strategies and governance. In the first phase of the pandemic, the Global Fund worked closely with ACT-Accelerator partners to ensure equitable allocation of the extremely limited volume of PCR diagnostics then available to LMICs, while working to secure greater production capacity, negotiate pricing and tackle implementation bottlenecks. Following the introduction of WHO-approved Ag-RDTs in September 2020, the Global Fund encouraged their deployment and the introduction of community-based testing and self-testing.
Alongside large-scale procurement and deployment of diagnostics, the Global Fund has also been supporting technical capacity building through Project STELLAR, supporting a group of 23 African countries in scaling-up COVID-19 testing, including wastewater testing, improving diagnostic governance and data management, and galvanizing longer term strengthening of laboratory systems, a key component of resilient and sustainable health systems.
In 2023, as the acute phase of the disease had passed and COVID-19 is becoming endemic in many countries, the priorities of implementing countries have shifted towards longer-term investments in health infrastructure and capacities for pandemic preparedness. To respond to counties’ needs, C19RM priorities have shifted to strengthening key components of an effective health system, especially laboratory systems, surveillance, human resources (including community health workers), supply chain management, oxygen and respiratory care, infection prevention and control (IPC), pandemic preparedness and response (PPR) and sustainable waste management. In addition, the Global Fund continues to work towards limiting the impact of COVID-19 on high-risk populations in LMICs through Test and Treat integrated service delivery models. Key activities include facilitating access to novel treatments and providing technical assistance to integrate treatment into existing public health infrastructure.
To learn more, visit the Global Fund’s C19RM page