What is the ACT Accelerator?
The Access to COVID-19 Tools (ACT) Accelerator was created after the outbreak of the SARS-COV-2 pandemic in 2020.
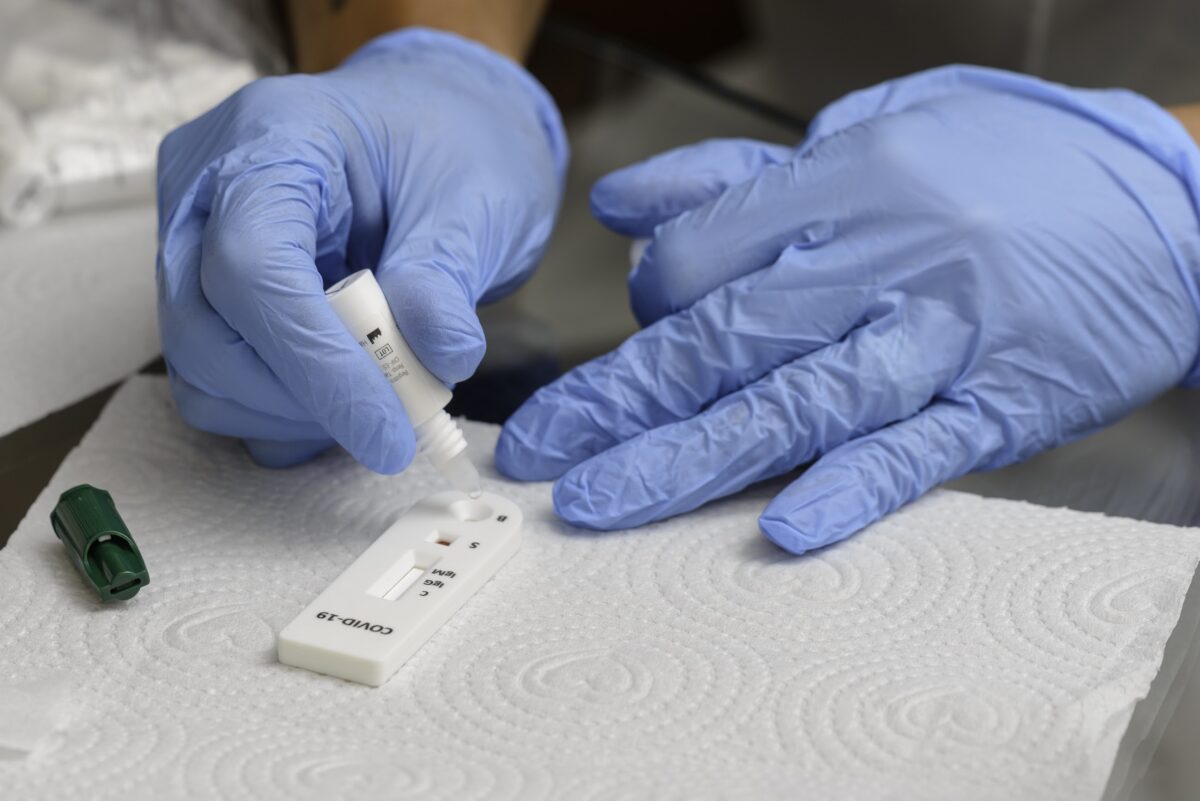
It is a global collaboration that uses existing public health infrastructure and expertise to accelerate the development and production of Covid-19 tests, treatments, and vaccines. It also focuses on providing equitable access to diagnostics and treatment.
The ACT Accelerator was launched in April 2020.
It has played a significant role in supporting the fasted and best coordinated global effort in history to fight a disease.
Its current focus is on scaling up access to Covid-19 tools worldwide.
Who are the convenors?
The ACT-Accelerator is co-convened by leading global health organizations.
It consists of three pillars and two or three partner agencies managing these.
What are the three pillars?
The three pillars of the ACT-Accelerator are the vaccines pillar, the diagnostics pillar, and the therapeutics pillar.
What does each pillar do?
The Vaccines Pillar has set a goal to rapidly rollout at least 2 billion vaccine doses in 2021 to high risk groups. It also has a goal to expand research and development.
Its third task is to identify new and emerging risks from variants of the SARS-COV2 virus.
The Diagnostics Pillar aims to identify new diagnostics and devliver 900 million high-quality tests by the end of 2021 to low- and low-middle income countries.
The Therapeutics Pillar promote research for effective treatments and ensure that countries optimize clinical care including the use of corticosteroids and medical oxygen for severe and critical patients. It also seeks to introduce new therapies and distribute up to 100 million treatment courses for populations in low and middle-income countries.
What does the Health Systems Connector do?
The Health Systems Connector (HSC) works across the three product pillars to identify and address bottlenecks in health systems worldwide and to enable the rollout of Covid-19 tools. The HSC also focuses on the rollout of personal protective equipment to health workers.
What is the role of the Access & Allocation workstream?
This workstream focuses on ensuring global equity and the allocation of Covid-19 resources. It also ensures that civil society and community engagement are integrated across all the pillars.